Our Mission
A revolutionary approach in brain retraction
The accessing of surgical sites within the brain requires retraction to gain access to the target site. The risk of retractor injury has been well documented. In fact, an estimated ten percent of skull base surgeries and five percent of aneurysm surgeries are complicated by brain infarction or contusion from retraction. Consequently, injury is often a result of direct pressure and local ischemia.
The most commonly used instruments in brain retraction procedures are ribbon or blade retractors, however neurosurgeons have a need for devices that provide better surgical outcomes. Increasingly the focus is on minimally invasive procedures that can improve post-operative quality of life through decreasing morbidity associated with conventional surgical procedures and reduce the length of patient hospitalization.
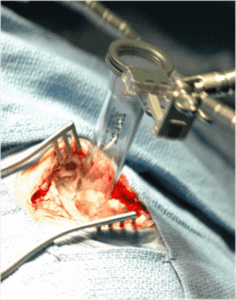
Vycor Medical’s ViewSite™ Brain Access System (VBAS™) is a neurosurgical device that enables safer access to specific targets within the brain, especially in procedures involving deep-seated lesions. VBAS was developed to address long-standing challenges in neurosurgery, where traditional retraction systems can inadvertently damage healthy brain tissue by exerting excess pressure on the soft tissue that is being retracted during surgical procedures.
Less brain tissue damage, less invasive
There is a lower risk of Ischemic complications and the procedure results in faster wound healing and a shorter patient recovery period; surgeon feedback also points to shorter OR time as there are no target shift issues through pulling, less consumables needed and greater ease of use.

Superior field of view and visibility

Better Access, Improved Working Channel
Compatible with Neuronavigation
The VBAS system is compatible with the most commonly used neuronavigation platforms and computer-guided technologies that help surgeons accurately reach the pre-identified target in real time. The neuronavigation pointer or probe is inserted into the cup at the tip of the VBAS introducer, and then locked in place by the VBAS Alignment Clip, with the pointer and VBAS effectively becoming one unit. The combination of the VBAS with neuronavigation provides the surgeon with a dynamic control of the visual field and stable retraction.
Previously Inoperable…Now Operable
“Her case would have been inoperable via a traditional surgery, because she was taking Avastin®, which delays surgical wound healing. The VBAS’ minimally invasive nature enabled the surgeon to gain access to the target through only a 3cm incision. The patient was discharged uneventfully and there were no issues regarding her wound.”
Daniel Prevedello, MD, Director of the Minimally Invasive Cranial Surgery Program, Ohio State University
Narayan Sundaresan, MD, Chief Neurosurgeon at Lincoln Medical Center, NY, and Professor at Mount Sinai Hospital, NYC
